Understanding Peripheral and Central Sensitization
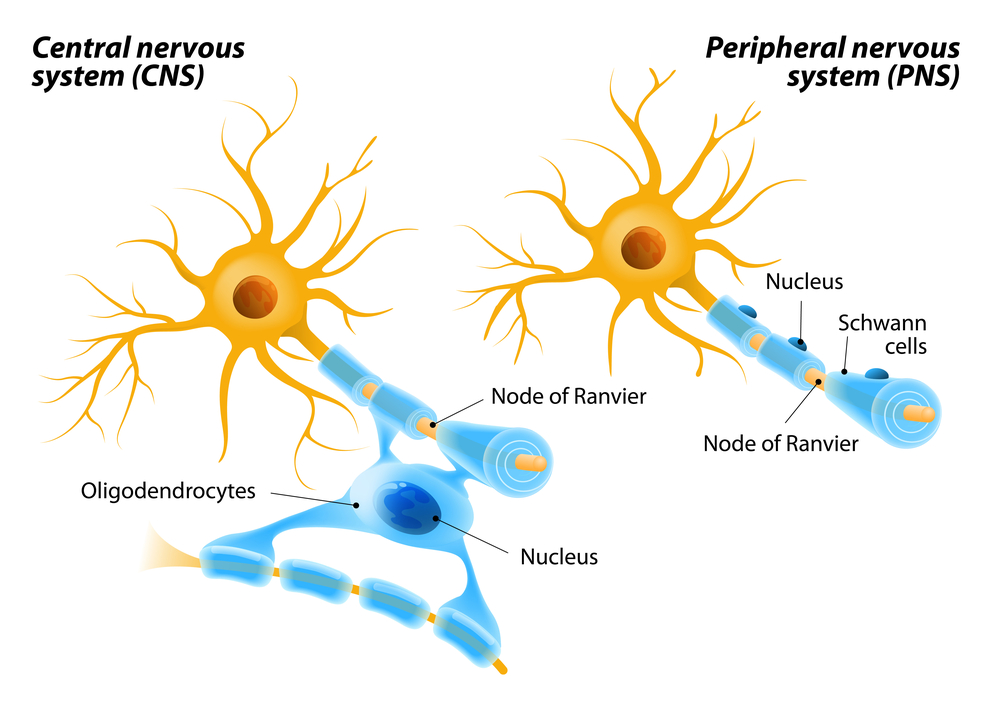
The human nervous system is an extremely complex network of nerve receptors, transmission fibers, gateways and, of course, the brain. In general, there are two distinct parts of the human nervous system: the central nervous system, which is comprised of the brain and spine, and the peripheral nervous system, which includes that network of nerves that transmits nerve impulses to the rest of the body.
One of the key purposes of the nervous system is to monitor the state of the human body. If an illness or injury occurs, then sensory receptors fire off a nerve impulse that indicates a part of the body has suffered damage. After traveling through the spinal circuits where there is some minor signal processing, this nerve impulse reaches the brain and is interpreted as pain.
Sensitization is a heightened sensitivity to stimuli that may occur normally in the central or peripheral nervous system, but this condition is also present in many chronic pain conditions. In pathological conditions, sensitization may produce pain stimuli even if no harmful events are occurring.
Peripheral Sensitization
The peripheral nervous system is divided into the somatic and autonomic nervous systems. The somatic nervous system delivers voluntary nerve impulses from the brain to other parts of the body including face and appendages. The autonomic nervous system is in control of involuntary physiological functions like digestion and heart rate.
The sensory nervous system is part of the somatic nervous system and transmits nerve signals from nociceptors throughout the body to the brain. Although some nerves are dedicated to either sensory or somatic transmission, many serve in both networks.
There is a normal sensitization response following an injury that is intended to help prevent additional harm. This sensitization results from a reduction in the stimuli threshold in the sensory nerve fibers. You may notice how tender the surrounding tissue becomes after an injury; this is the natural sensitization response.
In a pathological pain condition, however, peripheral nerves may produce pain signals in response to an innocuous stimuli (allodynia); produce an oversized pain response to a harmful stimuli (hyperalgesia); or produce pain without any stimuli at all. This is known as nociceptive pain which signifies that the internal mechanism of nerve signal transduction remains mostly intact.
When neurons become damaged and produced pain signals abnormally, this is designated as neuropathic pain. In healthy nerve cells, the stimulated sensory endings are where the nerve impulses are produced. However, in neuropathy, the impulse is generated where the damage to the nerve cell occurred, in essence, short circuiting the neuron.
Central Sensitization
Like peripheral sensitization, central sensitization also involves an increased response to nociceptors, although in this case, these are located in the spine and brain. Central nervous system nociceptors may become hypersensitive to stimuli; overly responsive to innocuous stimuli; or produce a pain response when not stimulated.
Unlike peripheral sensitization, however, central sensitization may also affect other senses. Many chronic pain patients with central sensitization issues may also experience sensitivity to light, sound and odors.
Central sensitization may also interfere with other cognitive functions like memory and concentration. Emotions like anxiety and depression may also be heightened if the central nervous system is sensitized. In some cases, this condition has also been associated with sick role behaviors like fatigue and malaise.
Although in some patients the cause of central sensitization may originate with a stroke or spinal cord injury, in many cases, there is no well-defined origin. Certain chronic pain patients may develop central sensitization as a result of injury to the peripheral nervous system. The exact mechanism of sensitization spread is unclear, but researchers have linked susceptibility to hereditary factors as well as a predisposition to anxiety. Patients who are more prone to stress are more likely to have a higher sensitivity to pain.
Therapies for Peripheral and Central Sensitization
It can be difficult to treat peripheral and central sensitization, but chronic pain can be managed given enough time and patient participation. Not all therapies will be effective for every patient suffering from sensitization issues, so it is often worthwhile to try a variety of treatment options while under the supervision of a pain specialist.
Among the sensitization therapies worth trying are
- Acetaminophen—this over-the-counter medication may inhibit central sensitization by reducing the effectiveness of the enzyme cyclooxygenase.
- Serotonin reuptake inhibitors—commonly prescribed medications like Prozac may not only mitigate depression and anxiety, but they may also inhibit central sensitization.
- Opioids—opioids act on opioid receptors in neurons found in the brain and block some of the pain impulses.
- Gabapentin—this drug inhibits signal transmission among neurons by binding to calcium channels that are instrumental to this mechanism.
- Cognitive retraining—because negative thought processes like anxiety may intensify pain symptoms, it is important to train chronic pain patients to alter their perception of pain. This may be accomplished by behavioral counseling, biofeedback or mindful meditation.
- Manual therapy—although primarily used to treat peripheral sensitization, massage therapy does boost endorphin production which, in turn, acts on central nervous system pain receptors.
- Transcranial magnetic stimulation—this therapy involves placing a coil of conducting wire upon the scalp and producing a series of brief magnetic pulses. TMS has helped patients with neuropathy, traumatic brain injury and migraines.
- Physical therapy—a vigorous physical therapy program has played an important role in managing peripheral and central sensitization for many chronic pain patients. These programs almost always include exercise and may be supplemented by ultrasound, TENS, or dry needling treatments as well.
- Acupuncture—although relatively unresearched by the medical community, acupuncture is gaining support due to the centuries of success in Asia as well as the minimal risks involved.
- Healthy diet—studies show that a strict diet may help with peripheral and central sensitization. You and your physician may need to perform an elimination study in which you consume a food that has potentially detrimental effects on your peripheral and central sensitization. If you react negatively to consuming the food, then you should eliminate it from your diet.
Article written by: Dr. Robert Moghim – CEO/Founder Colorado Pain Care
M.D. Disclaimer: The views expressed in this article are the personal views of Robert Moghim, M.D. and do not necessarily represent and are not intended to represent the views of the company or its employees. The information contained in this article does not constitute medical advice, nor does reading or accessing this information create a patient-provider relationship. Comments that you post will be shared with all visitors to this page. The comment feature is not governed by HIPAA and you should not post any of your private health information.



