Defeating Pain with Neurostimulation
For many people with chronic pain conditions like peripheral causalgia, complex regional pain syndrome or phantom limb pain, life is an agonizing ordeal. In many cases, chronic pain is an unrelenting condition that interferes with almost every aspect of daily life. Although there are many treatment options for these chronic pain conditions, they often come with serious side effects like opioid addiction, significant time investment or limited effectiveness.
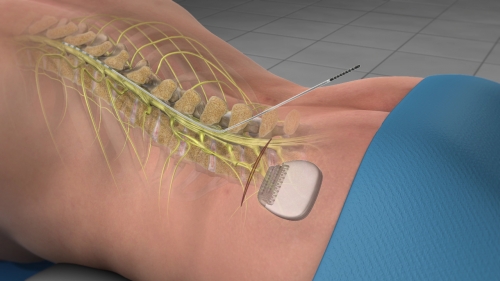
One of the most promising chronic pain therapies in recent years has been neurostimulation. Neurostimulation involves the stimulation of nerves in the spine or brain with electrical or magnetic fields. This modulation of nerves inhibits the normal transmission of pain impulses to the brain.
What Is Neurostimulation?
Although you may not have heard of the term neurostimulation, you may have heard of commonly used neurostimulation devices like TENS (transcutaneous electrical nerve stimulation) or Quell. Neurostimulation is becoming more popular among chronic pain patients as more physicians restrict the dispensation of opioid medications and recommend non-pharmacological alternatives.
Originally developed in 1967, neurostimulation was initially used to stimulate spinal cords. Spinal cord stimulation or SCS is a technique that requires electrical leads be placed beneath the skin and near the spinal cord. The leads are attached to a small pulse generator that produces mild electrical currents. These mild currents interfere with pain signals from the limbs or trunk, diminishing pain symptoms by up to 50 percent.
In modern neurostimulation devices, the entire mechanism may be implanted underneath the skin, or a radiofrequency power source may remain external if the amount of power needed is too high to sustain with an internalized battery. The current intensity may be adjusted by the patient through a remote control. Although surgical implantation is usually necessary for spinal cord stimulation, the procedure is currently only minimally invasive.
There are non-invasive forms of neurostimulation that include TENS or Quell, but these products usually only provide relief for milder chronic pain cases and only temporarily at that. TENS is usually available only through a physician’s or physical therapist’s office. Quell and similar neurostimulation products are available through retailers without a prescription and come with almost no side effects; if you are considering a more permanent neurostimulation solution, you may want to try one of these products first to see if you respond to this technique.
Who Is a Candidate for Neurostimulation?
Ultimately, candidates for neurostimulation procedures like spinal cord stimulation are patients who are most likely to respond positively to such a treatment. Patients with the following conditions are most likely to be considered for neurostimulation:
- Failed Back Syndrome (FBS)
- Radicular pain syndrome or radiculopathies
- Postlaminectomy pain
- Unsuccessful disk surgery
- Degenerative Disk Disease (DDD)/herniated disk pain
- Peripheral causalgia
- Epidural fibrosis
- Arachnoiditis or lumbar adhesive arachnoiditis
- Complex Regional Pain Syndrome (CRPS)
Not everyone with chronic pain is an ideal candidate for neurostimulation, but there is a relatively simple selection process. First of all, because neurostimulation is an invasive procedure, only patients who have tried more conservative therapies without success are considered. Candidates must exhibit no chemical dependencies and must pass a psychological standard.
Unlike other pain treatments, neurostimulation has a trial procedure that enables physicians to identify patients who respond positively to this kind of therapy. This trial involves temporarily placing two electrical leads just below the skin and running a light current. If the patient experiences some pain relief, then they are a viable candidate for a permanent neurostimulation procedure.
How Effective Is Neurostimulation for Pain Relief?
Neurostimulation has proven very successful for many chronic pain patients, but it doesn’t work for everyone. In one meta-study of spinal cord stimulation and peripheral nerve stimulation for chronic pain, it was found that neurostimulation was generally quite effective. Among 15 SCS trials, nine showed improvement in pain symptoms and two out of the 7 PNS studies reported significant pain relief among study participants.
There is some debate as to how selective physicians should be with potential candidates. Some medical authorities argue that due to the relative effectiveness and low cost of the neurostimulation products and procedure, more people should be considered for candidacy.
Most importantly, neurostimulation may have a radically life-altering effect for patients in severe, chronic pain. New advances in neurostimulation like dorsal root ganglion targeting promise that this pain therapy will only improve in effectiveness in the years to come. There is also mounting hope that Deep Brain Stimulation, which has only been used to treat movement or psychiatric disorders previously, could prove successful in pain management.
Benefits and Disadvantages of Neurostimulation
There are many potential benefits from neurostimulation, but the most important is its ability to produce long-term pain relief. According to the Neuromodulation Appropriateness Consensus Committee, 93 percent of patients with a spinal cord stimulator experienced some pain relief if the stimulator was implanted within three years of a failed back surgery. However, this dropped to 9 percent if there was a span of more than 12 years since the failed back surgery.
Furthermore, SCS implantation has proven more cost effective than traditional pain therapies in the long term. It has been estimated that SCS could save from $28,000 to $39,000 over a five-year period.
It is also important to be aware of potential complications. Studies show that there is a 30 to 40 percent chance of lead breakage, lead migration or other device complication that may require a revision procedure. There is a comparable and minimal rate of serious complications like spinal cord injury as with any other major surgery.
The NACC reports that there is a 4 to 10 percent risk of infection at the implant site. There is a 2.5 percent chance of fluid accumulation at the site of the pulse generator, while there is a 0.3 percent risk of a spinal cord lesion forming. Among 0.3 percent of patients following a spinal cord stimulator implantation began experiencing headaches or pain at the device site.
Many patients also report that pain relief diminish over time, necessitating an increase in current amplitude. This may be avoided by frequency modulation.
Article written by: Dr. Robert Moghim – CEO/Founder Colorado Pain Care
M.D. Disclaimer: The views expressed in this article are the personal views of Robert Moghim, M.D. and do not necessarily represent and are not intended to represent the views of the company or its employees. The information contained in this article does not constitute medical advice, nor does reading or accessing this information create a patient-provider relationship. Comments that you post will be shared with all visitors to this page. The comment feature is not governed by HIPAA and you should not post any of your private health information.



